EXPLORING HEMOGLOBIN TOXICITY AFTER INTRACRANIAL BLEEDING
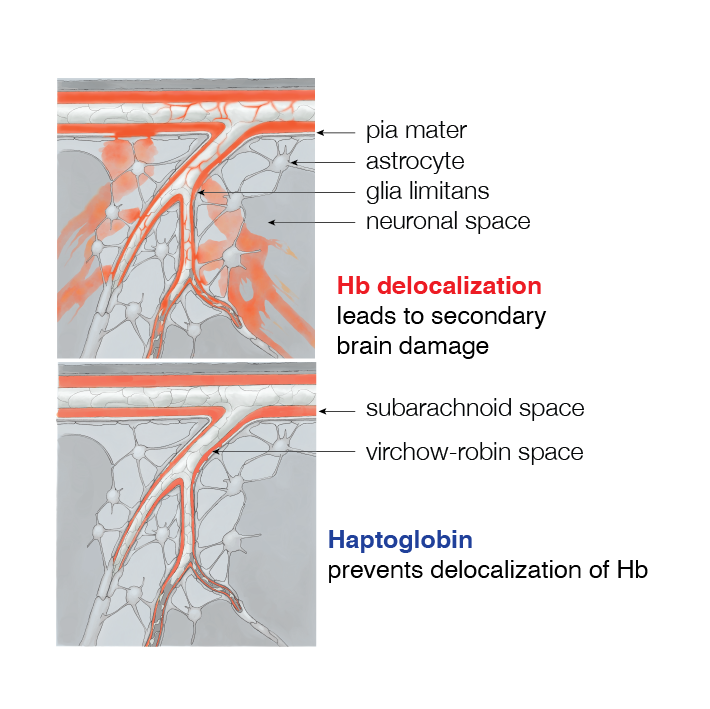
Among all conditions of cell-free hemoglobin exposures, intracranial hemorrhage with subsequent erythrolysis may be the most devastating. During systemic hemolysis, cell-free hemoglobin is rapidly cleared by renal filtration, limiting tissue exposure. In contrast, erythrolysis after intracranial bleeding leads to unchecked accumulation of Hb, heme, and iron in cerebrospinal fluid and within the brain parenchyma.
We found in patients with subarachnoid hemorrhage, rodents, and large animal models that cell-free Hb can cause secondary brain damage after bleeding, and we have provided proof-of-concept that the toxicity of cell-free hemoglobin in the brain can be neutralized by the administration of the scavenger proteins into the cerebrospinal fluid.
The tremendous unmet medical need for novel therapeutics in this field led us to initiate a preclinical drug development program conquering secondary brain damage in patients with intracranial bleeding.
Hemoglobin Toxicity in the brain
(adapted from Buehler PW et al., 2020 and Hugelshofer M et al., 2019)
READINGS
Spatial transcriptome analysis defines heme as a hemopexin-targetable inflammatoxin in the brain
Buzzi RM, Akeret K, Schwendinger N, Klohs J, Vallelian F, Hugelshofer M, Schaer DJ. (2022).
Free Radical Biology and Medicine.
Abstract
After intracranial hemorrhage, heme is released from cell-free hemoglobin. This red blood cell component may drive secondary brain injury at the hematoma‒brain interface. This study aimed to generate a spatially resolved map of transcriptome-wide gene expression changes in the heme-exposed brain and to define the potential therapeutic activity of the heme-binding protein, hemopexin. We stereotactically injected saline, heme, or heme‒hemopexin into the striatum of C57BL/6J mice. After 24 h, we elucidated the two-dimensional spatial transcriptome by sequencing 21760 tissue-covered features, at a mean transcript coverage of 3849 genes per feature. In parallel, we studied the extravasation of systemically administered fluorescein isothiocyanate labeled (FITC)-dextran, magnetic resonance imaging features indicative of focal edema and perfusion, and neurological functions as translational correlates of heme toxicity. We defined a cerebral heme-response signature by performing bidimensional differential gene expression analysis, based on unsupervised clustering and manual segmentation of sequenced features. Heme exerted a consistent and dose-dependent proinflammatory activity in the brain, which occurred at minimal exposures, below the toxicity threshold for the induction of vascular leakage. We found dose-dependent regional divergence of proinflammatory heme signaling pathways, consistent with reactive astrocytosis and microglial activation. Co-injection of heme with hemopexin attenuated heme-induced gene expression changes and preserved the homeostatic microglia signature. Hemopexin also prevented heme-induced disruption of the blood‒brain barrier and radiological and functional signals of heme injury in the brain. In conclusion, we defined heme as a potent inflammatoxin that may drive secondary brain injury after intracerebral hemorrhage. Co-administration of hemopexin attenuated the heme-derived toxic effects on a molecular, cellular, and functional level, suggesting a translational therapeutic strategy.
Cerebrospinal fluid hemoglobin drives subarachnoid hemorrhage-related secondary brain injury
Akeret K, Buzzi RM, Schaer CA, Thomson BR, Vallelian F, Wang S, Willms J, Sebök M, Held U, Deuel JW, Humar R, Regli L, Keller E, Hugelshofer M, Schaer DJ. (2021).
Journal of Cerebral Blood Flow & Metabolism.
https://doi.org/10.1177/0271678X211020629
Abstract
Secondary brain injury after aneurysmal subarachnoid hemorrhage (SAH-SBI) contributes to poor outcomes in patients after rupture of an intracranial aneurysm. The lack of diagnostic biomarkers and novel drug targets represent an unmet need. The aim of this study was to investigate the clinical and pathophysiological association between cerebrospinal fluid hemoglobin (CSF-Hb) and SAH-SBI. In a cohort of 47 patients, we collected daily CSF-samples within 14 days after aneurysm rupture. There was very strong evidence for a positive association between spectrophotometrically determined CSF-Hb and SAH-SBI. The accuracy of CSF-Hb to monitor for SAH-SBI markedly exceeded that of established methods (AUC: 0.89 [0.85-0.92]). Temporal proteome analysis revealed erythrolysis accompanied by an adaptive macrophage response as the two dominant biological processes in the CSF-space after aneurysm rupture. Ex-vivo experiments on the vasoconstrictive and oxidative potential of Hb revealed critical inflection points overlapping CSF-Hb thresholds in patients with SAH-SBI. Selective depletion and in-solution neutralization by haptoglobin or hemopexin efficiently attenuated the vasoconstrictive and lipid peroxidation activities of CSF-Hb. Collectively, the clinical association between high CSF-Hb levels and SAH-SBI, the underlying pathophysiological rationale, and the favorable effects of haptoglobin and hemopexin in ex-vivo experiments position CSF-Hb as a highly attractive biomarker and potential drug target.
Haptoglobin Therapeutics and Compartmentalization of Cell-Free Hemoglobin Toxicity
Buehler PW, Humar R, Schaer DJ. (2020).
Trends in Molecular Medicine.
Abstract
Haptoglobin administration into the subarachnoid space prevents hemoglobin-induced cerebral vasospasm
Michael Hugelshofer, Raphael M. Buzzi, Christian A. Schaer, Henning Richter, Kevin Akeret, Vania Anagnostakou, Leila Mahmoudi, Raphael Vaccani, Florence Vallelian, Jeremy W. Deuel, Peter W. Kronen, Zsolt Kulcsar, Luca Regli, Jin Hyen Baek, Ivan S. Pires, Andre F. Palmer, Matthias Dennler, Rok Humar, Paul W. Buehler, Patrick R. Kircher, Emanuela Keller, Dominik J. Schaer. (2019).
The Journal of clinical investigation, 129(12).
https://doi.org/10.1172/JCI130630
Abstract
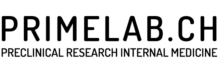
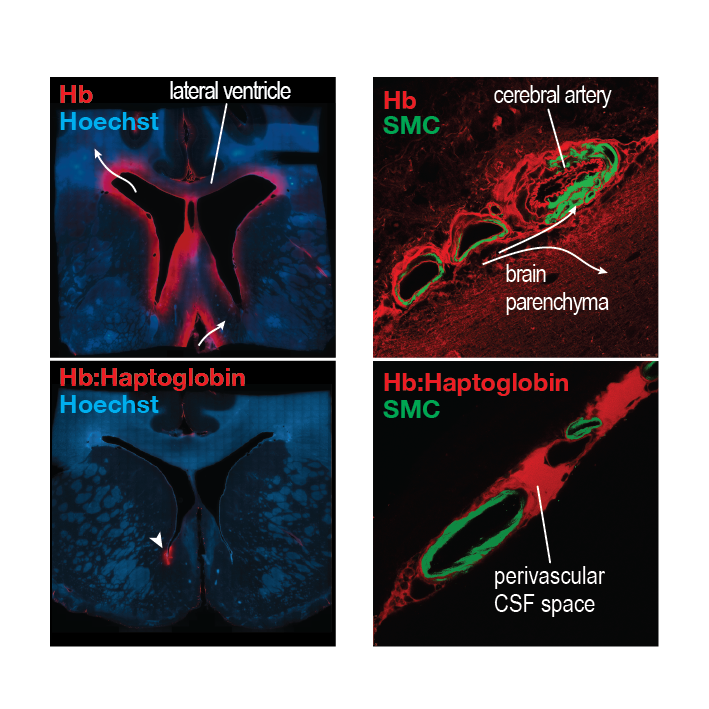
Delayed ischemic neurological deficit (DIND) is a major driver of adverse outcomes in patients with aneurysmal subarachnoid hemorrhage (aSAH), defining an unmet need for therapeutic development. Cell-free hemoglobin that is released from erythrocytes into the cerebrospinal fluid (CSF) is suggested to cause vasoconstriction and neuronal toxicity, and correlates with the occurrence of DIND. Cell-free hemoglobin in the CSF of patients with aSAH disrupted dilatory NO signaling ex vivo in cerebral arteries, which shifted vascular tone balance from dilation to constriction. We found that selective removal of hemoglobin from patient CSF with a haptoglobin-affinity column or its sequestration in a soluble hemoglobin-haptoglobin complex was sufficient to restore physiological vascular responses. In a sheep model, administration of haptoglobin into the CSF inhibited hemoglobin-induced cerebral vasospasm and preserved vascular NO signaling. We identified 2 pathways of hemoglobin delocalization from CSF into the brain parenchyma and into the NO-sensitive compartment of small cerebral arteries. Both pathways were critical for hemoglobin toxicity and were interrupted by the large hemoglobin-haptoglobin complex that inhibited spatial requirements for hemoglobin reactions with NO in tissues. Collectively, our data show that compartmentalization of hemoglobin by haptoglobin provides a novel framework for innovation aimed at reducing hemoglobin-driven neurological damage after subarachnoid bleeding.
Cell-Free Oxyhemoglobin in Cerebrospinal Fluid After Aneurysmal Subarachnoid Hemorrhage: Biomarker and Potential Therapeutic Target
Hugelshofer M, Sikorski CM, Seule M, Deuel J, Muroi CI, Seboek M, Akeret K, Buzzi R, Regli L, Schaer DJ, Keller E. (2018).
World Neurosurgery, 120, e660-e666.
https://doi.org/10.1016/j.wneu.2018.08.141